Similar to James, I also plan on going into the
medical field. Much of what I have to
say is similar, as our two fields coincide, but I will attempt to make my post
as unique as I can, or at least give it a different flavor through my own
voice.
I am still ambivalent and oscillating as to what
exact study I am going to devote my career to, but I have narrowed the choices
down mainly to pharmacy and surgery (and also maybe neurology). Though the realms are quite different in
terms of prescribing and physically applying learned medical skills, the
rhetoric employed is nearly identical.
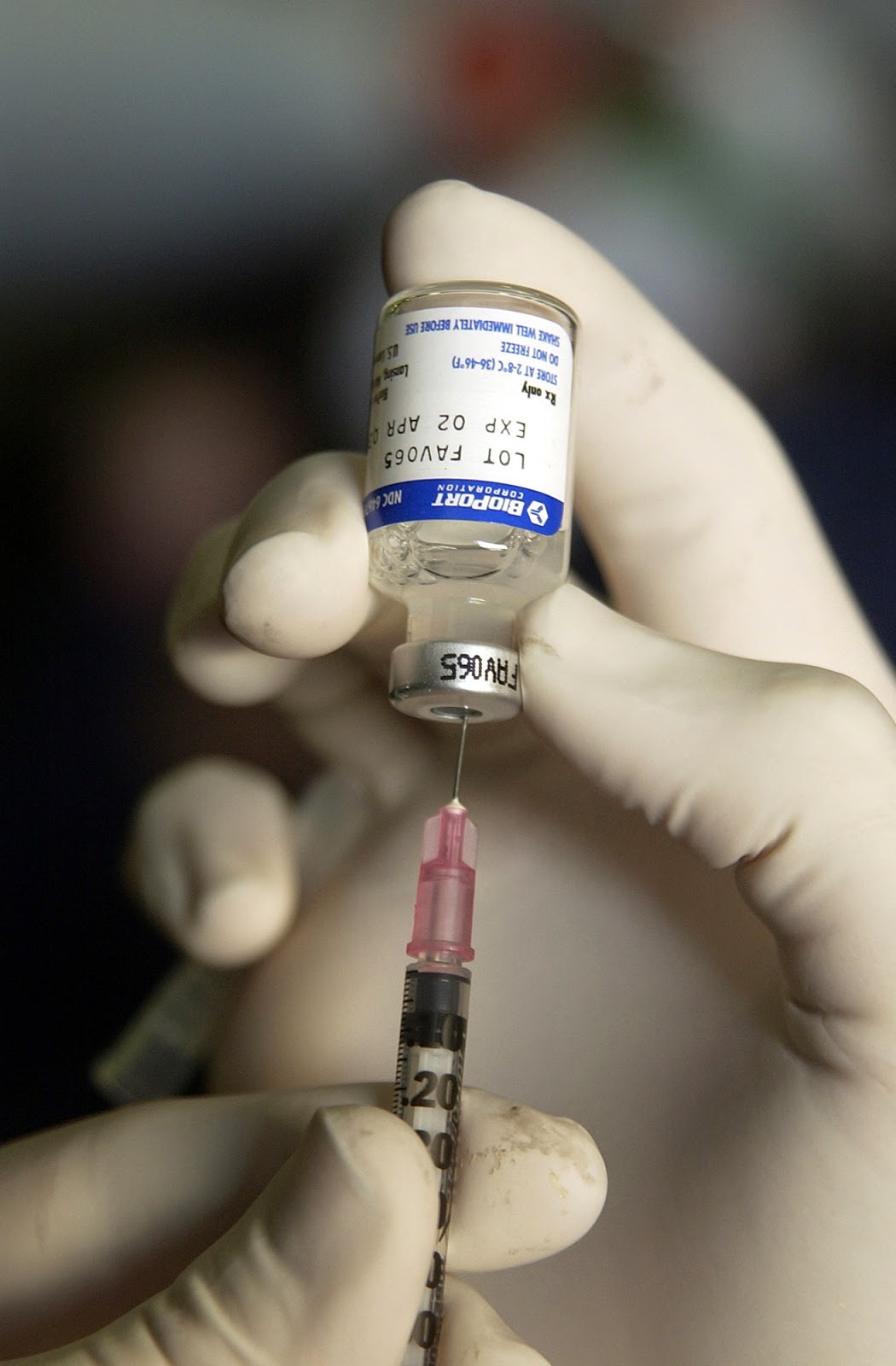 |
| One must know what to put in the syringe, and where best to put the syringe, while also convincing the patient to accept the syringe. |
As a physician or surgeon, communication first takes
place in the office or in the operation room, depending on the patient's
current circumstances being dire, or slightly less so. Either way, be it an emergency or a routine
checkup, the patient must be convinced via oral or written reasoning and information
as to whether or not to go through with what the doctor professes is
"best." This can be an easy
process at times, as the authoritative presence of someone who has spent a
large portion of their life to study and practice bears much weight. Conversely, a stubborn or skeptical patient
might require substantial counseling before accepting or rejecting aid. The outcome of this decision is in part
determined by urgency and the gravity of the patient's condition, but much of
the time is also heavily reliant on how effective the doctor is in
persuasion.
"To take this medicine or that medicine—or no
medicine," or "to go under the knife and radiation, or risk it"
are some of the dilemmas patients must acquire an opinion on. "Is it worth it," and "what is 'it?'" Before making a decision to heed or dismiss
the advice of the doctor, the patient must better understand the nature of
their own condition, a worrisome need readily assuaged by said physician or
surgeon.
 |
| Take the right one and you live, but take the wrong one and you die. Better ask the doctor first. |
In theory, the doctor is the more knowledgeable of
the two with regards to the patient, no doubt due to numerous years of learning
and practice before actual application even begins, but this is not always the
case. In general, yes, the patient feels
a sense of inferiority to the doctor, or possibly just respect for the medical
position, but this does often lead to excessive pride in the doctor. This "God Complex," as James put
it, is a force that must be monitored.
In my own personal experience, I had a medical
tragedy that kept me out of school for two years (and continues to inhibit my
success in academics even now). Fearing
for my health and even my life, I consulted a doctor for their professional
diagnosis. Going into the meeting, I had
a theory as to what had happened to me, but the doctor disregarded the thought
and labeled it "impossible." Putting
me through all the motions for the tests that he thought I needed to go through, the results concluded that
nothing was wrong with me—a self-fulfilling prophecy that deeply offended
me. My proposition was to look into a
second, "impossibly" rare scenario, but I was merely stuck with a
massive painkiller shot and sent home.
 |
| Though the Tenth Doctor might be experienced, I do not think that he has the appropriate "experience" for solving most medical issues, nor of harboring the corresponding ethos. |
Months later, I was still unable to properly
function, and after attempting to return to school, was forced to go back home
and seek further medical assistance.
Something was wrong with me,
and after meeting with another, more receptive doctor, we found that I indeed
had suffered the exact condition that I had suspected and feared.
To make a long story short, a doctor must make
excellent use of logos in assessing issues in a patient and providing a train
of thought leading said patient to accepting help. This is not all, however, because though the
doctor must exercise skillful epideictic oratory (and even judicial oratory to
demonstrate prior experiences and results), they must do it in a way so as not
to dissuade the patient from
accepting the physician's or surgeon's ethos.
Additionally, in order to be the most effective doctor, one must be
willing to listen to the plea of the patient, as neither of the two parties are
operating or prescribing for themselves.
Without a proper connection of minds under mutual respect, a doctor's
rhetoric can still fail him or her. Looking
back at my own interest in this field and my unfortunate, but eye-opening
event, I wish to pursue the path of biology with a wiser gait.
You make many good points, especially regarding the necessity of mutual respect. Rhetoric takes an unselfish turn when the doctor must employ it to truly serve and help the patient, rather than achieve his or her purposes.
ReplyDeleteMy mom has worked among doctors for over 20 years, she always says that the best doctors are compassionate and caring people. She has often said that there need to be more doctors who really care, not to the point where the professional patient-physician relationship is breached or the doctor becomes too attached, but to the point where the patient can actually trust and really heal. I think that's probably something that you were able to see with your health struggles that you shared.
ReplyDeleteGreat insights Thomas.
ReplyDeleteI think its extremely difficult to persuade someone if they have already made up their mind about something. I think this shows the two sides of rhetoric that the ancient greeks and romans both feared and respected. If used correctly, rhetoric can be a force for much good and progress, if used incorrectly it can give way to selfish and prideful ends.
I wish you the best of luck as you face your medical condition.
Thank you for your thoughts.
Delete